Hand Surgery
Our surgeons are fully qualified hand surgeons and members of the British Society for Surgery of the Hand. We offer hand surgery for a range of conditions, which include:
1. Ganglions
Although ganglions can arise from any joint or tendon tunnel, there are four common locations in the hand and wrist - in the middle of the back of the wrist; on the front of the wrist at the base of the thumb; at the base of a finger, and on the back of a finger end-joint.

Ganglions occur when synovial fluid leaks out of a joint or tendon tunnel and forms a swelling under the skin, although the cause of these leaks is not known. In some cases ganglions are painful, in others they are not.
What surgery is available, and what techniques are involved?
Ganglions are harmless and can be safely left alone. However, for people who want to get rid of a ganglion, treatments options vary depending on the location of the swelling and the symptoms it is causing.
The liquid contents of a ganglion can be removed with a needle (a procedure known as aspiration). However, the most definitive treatment is the surgical removal, or excision, or the ganglion in its entirety.
What can I expect as a patient?
Surgery can usually be done under local anaesthetic, with numbing injections which avoid the need for general anaesthetic. The ganglion is then excised. Removal of a ganglion close to the nail involves tracing it down to the joint and, in most cases, removing a small bone-spike. There is also often a shortage of skin in this part of the hand, which is best treated by moving skin from further down the finger, using a local flap.
The post-surgery scar is usually inconspicuous, but may become red and thick especially on the front of the wrist. Ganglions are known to recur on occasions, but can be removed again, still with a good chance of success. As with all operations on the hand, there is a small possibility of unexpected stiffness, swelling or pain requiring physiotherapy or other treatment.
Following the removal of a ganglion from the wrist, a bulky dressing or plaster splint will be applied. You will be encouraged to move the fingers regularly to avoid stiffness, and you will be able to move the wrist after 10-14 days. This might need to be supervised by a hand therapist. The usual recovery time following ganglion surgery ranges from two-to-three weeks for a small finger cyst, to six-to-eight weeks for wrist ganglions.
2. Carpal Tunnel Syndrome
Carpal tunnel syndrome is a condition caused by mechanical interference with the median nerve in the wrist. This large nerve provides feeling to the thumb, index and middle fingers and half of the ring finger. It also provides power to the small muscles at the base of the thumb. The compression is relieved when the transverse carpal ligament is divided in carpal tunnel release.
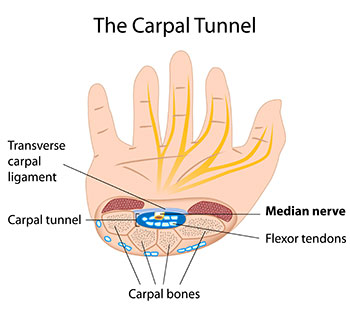
The median nerve enters the hand from the forearm, passing beneath a tough ligament (known as the transverse carpal ligament) that runs across the wrist. For reasons that are poorly understood, this nerve can become squeezed, either because the contents of the tunnel beneath the ligament swell, or because the size of the tunnel decreases. 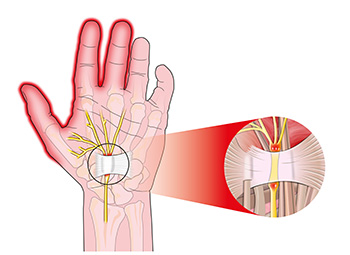 This squeezing of the nerve causes tingling in the fingers, often accompanied by numbness. These sensations are usually worse at night, and often wake a patient from sleep. Pain can occur later on in the condition and can be felt in the hand, forearm or even in the upper arm and shoulder.
This squeezing of the nerve causes tingling in the fingers, often accompanied by numbness. These sensations are usually worse at night, and often wake a patient from sleep. Pain can occur later on in the condition and can be felt in the hand, forearm or even in the upper arm and shoulder.
What surgery is available, and what techniques are involved?
Surgery to treat Carpal Tunnel Syndrome is simple and generally effective. It involves dividing the carpal ligament to allow it to relax and relieve the pressure on the nerve. This can be done in a number of ways, and a surgeon will outline the course of action most suitable to you.
Splinting of the wrist and steroid injections are also available treatment options, but surgery is the most reliable.
What should I expect as a patient?
The operation usually only takes a few minutes, with a patient having a local anaesthetic and discharged immediately afterwards. All that is usually required is the application of a dressing over the short scar at the wrist.
The results of this operation are usually good. Pain is almost always immediately relieved, and the tingling also subsides. If the hand has been affected for a long time, the numbness may persist for many weeks, and any loss of muscle bulk that has occurred is unlikely to improve.
As with all operations, procedures and outcomes vary from case to case. There can be occasional complications in Carpal Tunnel surgery, including unexpected bleeding, wound infection and lumpy or painful scars, but by and large this operation is simple, safe and highly successful.
3. Arthitis
The main joint at the base of the thumb is called the trapeziometacarpal joint. This joint carries a lot of force when the thumb is used, yet allows for a complex range of movements, including rotation. It is this load-bearing and movement that causes the wear and tear that brings on osteoarthritis.

Osteoarthritis can cause aching, especially between the thumb and the side of the index finger. The pain may lead to a sense of weakness when you pinch or grip. Actions such as opening the lid of a jar, or turning a key in a door, can be painful and difficult. The base of the thumb may become swollen and may crunch audibly during certain movements. It may also become misshapen. It is this pain and disability that often encourages people to seek surgical interventions.
What surgery is available, and what techniques are involved?
Before surgery is pursued, other treatments such as thumb splints or steroid injections may be carried out. If these treatments fail to support the thumb or reduce the pain, then surgery may be considered. The options include:
Joint stabilisation: involves either realignment of the bone or ligament reconstruction using a tendon; suitable only for a minority of patients who have an unstable joint but little damage to the surfaces of the joints.
Trapeziectomy: involves the complete removal of the trapezium bone; recommended if the joint above or below this bone are affected by arthritis. Some surgeons fill the gap left by the bone, with adjacent tissue.
Trapeziectomy with ligament reconstruction: performed if there are concerns that the thumb appears too slack to sit securely in the new joint created by the removal of the bone.
Arthrodesis: fusion surgery, which is normally reserved for younger patients; has the disadvantage of stiffening the thumb.
What can I expect as a patient?
Trapeziectomy is the most commonly performed surgical operation for osteoarthritis of the thumb. The operation is usually performed under general anaesthetic, supplemented by local anaesthetic. As a patient, you will need to stay in hospital for one or two nights after the operation. It will leave a scar on the back of your hand, and a bulky dressing to protect it. In the days following the operation, hand elevation is very important to prevent swelling and stiffness.
Stitches are usually removed at around two weeks after the operation, and the plaster may be changed for a lighter weight splint, which you will need to wear for up to six weeks. From about four weeks you can begin exercising the hand, using techniques passed on by a hand therapist. It normally takes six-to-nine months for strength in your thumb and hand to return, but improvement is usually steady. Although your strength in this area may never be as good as it was, most patients notice significant pain reduction.
Infection can occur, and severe stiffness can affect about 5% of patients.
4. Dupuytrens Contracture
The disease first makes its appearance as a small lump in the palm. Over time, this lump may form a cord of tissue that runs from the palm to the finger. After a while, this cord begins to shrink, drawing the finger into a clawed position. This is the contracture, and as it progresses the nuisance and disability associated with the condition worsens.

Often hereditary, the condition can take years to develop, but as a general rule, you should seek medical advice if you are unable to place the palm of your hand down flat on a tabletop.
What surgery is available, and what techniques are involved?
Surgery is the only treatment available for Dupuytren’s Contracture. In mild cases, the contracture can be corrected by creating a zigzag scar, known as a z-plasty, across the surface of the palm and finger; through this scar the diseased tissue is removed and the joint is freed. The zigzag shape also prevents the scar from shrinking and affecting finger flexibility. Following surgery the wound is closed, although elements of the scar may be left open to allow the blood to drain away.
In more complex cases it can also be necessary to remove the overlying skin and replace it with a skin graft taken from either the inner part of the arm or from the groin.
What should I expect as a patient?
Patients are operated on using local or general anaesthetic, and surgery takes between 30 minutes to two hours. After surgery a dressing is applied and the hand should be rested for one week in a splint or cast. Most patients are able to drive again within 10 days of their operation.
You should be able to leave hospital on the same day as the operation. You will be seen again after a week or so to have your dressings changed, and then after two weeks to have your stitches removed. The surgery is usually effective, but sometimes does not bring about a completee correction. Possible complications include poor wound healing, incomplete correction, stiffness and recurrence of the contracture.